OLIF and XLIF are minimally invasive “lateral” lumbar fusion approaches. They share goals (decompress, correct alignment, and stabilize) but differ in the anatomical corridor, the complication profile, and some recovery timelines. This guide, in plain language, explains when each technique is considered, how the problem is diagnosed, what alternatives exist, realistic benefits and risks, and when to seek emergency care.
- Practical 9-point comparison: anatomy, treatable levels, postoperative pain, typical complications, and return to work.
- What tests you really need before deciding—and when surgery is not advised.
- Non-surgical options and other techniques (endoscopy, TLIF/ALIF) with their pros and cons.
- Final checklist to talk with your specialist without forgetting anything important.
1. What are OLIF and XLIF?
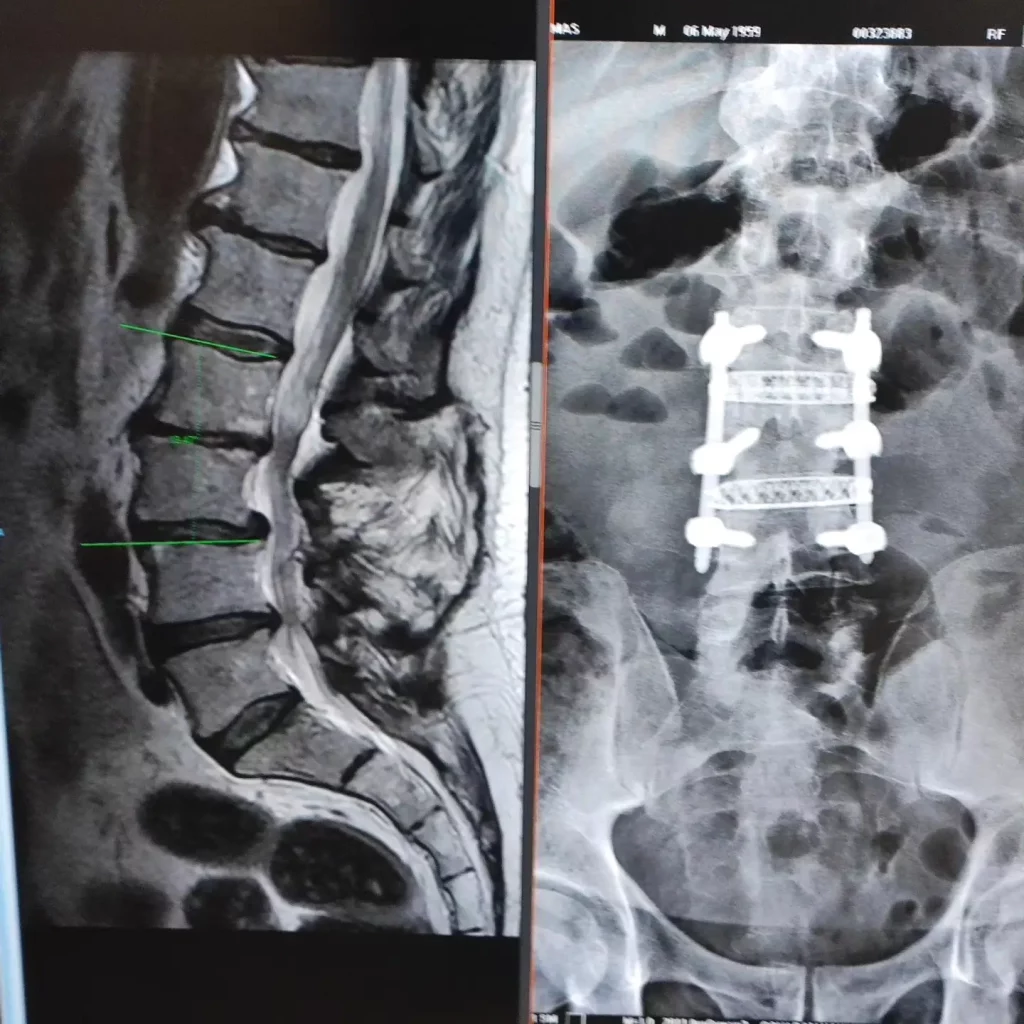
They are two variants of “lateral” lumbar fusion—minimally invasive techniques that place an interbody implant (cage) between two vertebrae to restore disc height, indirectly decompress the nerves, and improve alignment. In XLIF the access is transpsoas (through the psoas muscle). In OLIF it is anterior to the psoas, passing in front of this muscle and behind the peritoneum.
2. Symptoms and indications
Considered for mechanical low back pain with or without leg pain from foraminal compression, foraminal stenosis, and certain deformities or degenerative spondylolisthesis when well-executed conservative care has failed. It may also be considered in revision surgery or when a classic posterior approach would add more tissue disruption.
3. Diagnosis: useful tests (and which add little)
- History and neurological exam: identify the level and likely pain generator.
- MRI: test of choice to assess discs, facets, and neural compromise.
- Dynamic X-rays (flexion/extension): detect instability when suspected.
- CT: useful for screw planning or reviewing prior surgeries.
- Electromyography: reserved for diagnostic uncertainty or to distinguish peripheral pathology.
Do not chain tests if results won’t change management. Decisions are based on the sum of clinical picture and imaging—not on how “severe” the MRI looks.
4. The 9 key differences between OLIF and XLIF
- Anatomical corridor: XLIF traverses the psoas; OLIF passes in front of it. This shapes the typical complication profile.
- Psoas-related symptoms: after XLIF there may be transient hip-flexion weakness or tingling on the anterior thigh. In OLIF this is less common because the psoas is not traversed.
- Lumbar sympathetic chain: in OLIF there is a risk of sympathetic chain irritation (warmth or unilateral leg sweating) if retraction is prolonged; minimized with careful technique.
- Treatable levels: both address L2–L5 reliably; L4–L5 is more “demanding” due to plexus and vessel anatomy. L5–S1 usually requires other techniques (due to vessel position and the iliac crest).
- Alignment correction: restoration of height and segmental lordosis is comparable; cage size and adequate release are key—not just the approach.
- Indirect decompression: by restoring disc height, the foramen enlarges. If there is frank posterior compression (severe central stenosis), it is sometimes combined with direct decompression.
- Bleeding and postoperative pain: both are lower than with traditional open approaches; OLIF may result in less muscle discomfort by avoiding traversal of the psoas.
- Neurologic vs vascular events: XLIF has more transient neurologic events (psoas/plexus). OLIF has more sympathetic or rare vascular events; overall rates are low in experienced hands.
- Learning curve and team: require 3D planning and intraoperative imaging; an experienced team reduces complications and shortens times.
5. Non-surgical alternatives
- Education and exercise: lumbopelvic strength and motor-control program.
- Judicious analgesics: avoid chronic opioids.
- Physical therapy: manual therapy integrated into an active plan.
- Injections: temporary relief in selected cases (epidural, facet, sacroiliac).
The goal is to improve function and quality of life; many people avoid surgery with a well-executed plan.
6. Surgical alternatives and how they compare
- Endoscopy/microsurgical decompression: useful if the main problem is neural compression without instability.
- TLIF/PLIF (posterior): allow direct decompression and fusion from the back; more muscular manipulation.
- ALIF (anterior L5–S1): excellent for lordosis and foraminal height; requires a team with vascular experience.
The choice depends on anatomy, affected level, symptoms, and goals (radicular pain, instability, alignment correction).
7. Expected benefits and risks/adverse effects
Benefits
- Reduced radicular pain and improved function by enlarging the foramina.
- Faster recovery and less bleeding versus traditional open surgery.
- Possible alignment correction and prevention of disc collapse.
Risks
- Common to any fusion: infection, thrombosis, bleeding, nerve injury, pseudarthrosis, persistent pain.
- XLIF: transient hip-flexion weakness, anterior thigh paresthesias, femoral plexus irritation.
- OLIF: sympathetic chain irritation (temperature/sweating changes in the leg) and, rarely, vascular injury.
Serious complication rates are low with proper selection and an experienced team—but never zero.
8. Practical referral criteria
- Meaningful pain and functional limitation after 6–12 weeks of well-executed conservative care.
- Clear clinical–radiologic correlation (level and side).
- Progressive neurologic deficit or progressing deformity.
9. Realistic recovery timelines
- Daily life: early ambulation and basic tasks within a few days if recovery is favorable.
- Work: desk work in 2–6 weeks; physical jobs, 6–12 weeks or longer depending on demands and progress.
- Rehabilitation: a structured program for strength, mobility, and motor control accelerates return.
Timelines depend more on your baseline status, comorbidities, and activity type than on choosing OLIF or XLIF.
10. When to go to the emergency department
- Progressive loss of strength or marked sensation in the legs.
- High fever with disproportionate low back pain.
- Urinary/bowel changes or “saddle” anesthesia.
11. Myths and realities
- “A severe MRI forces surgery”: treat the person, not the image.
- “OLIF is always better than XLIF (or vice versa)”: it depends on anatomy and the goal.
- “After fusion I won’t move the same”: most people return to activity with good function if rehabilitation is done.
12. Frequently asked questions
Which hurts less, OLIF or XLIF?
Both aim to minimize pain and bleeding. XLIF may cause transient psoas-related symptoms; in OLIF they are less likely because the psoas is not traversed.
Can it be done at L5–S1?
It’s usually not the ideal level for lateral approaches; ALIF or other options are often considered.
Are they suitable for severe central stenosis?
They can help via indirect decompression, but with frank central compression a direct decompression is usually added.
How long does the implant last?
Fusion seeks a stable bony union. Durability depends on consolidation and factors like bone density, technique, and rehabilitation.
Will I be able to play sports?
In most people, yes—with guided progression. High-impact or maximal loads are reintroduced gradually according to progress.
What if the pain persists?
The cause is reassessed (nerve, facet, sacroiliac joint, hip) and the status of the fusion. Sometimes coexisting, treatable pain sources are present.
13. Glossary
- OLIF: oblique lumbar interbody fusion, access in front of the psoas.
- XLIF: extreme lateral lumbar interbody fusion, access through the psoas.
- Psoas: hip flexor muscle; near the femoral plexus.
- Sympathetic chain: nerve fibers regulating functions such as sweating and skin temperature.
- Indirect decompression: nerve relief by restoring disc/foraminal height.
- Pseudarthrosis: failure of fusion to consolidate.
References
- Dr. Vicenç Gilete – Neurosurgeon. https://complexspineinstitute.com/en/complex-spine-institute/en/institute/#medical_team
- Dr. Augusto Covaro – Orthopedic and trauma surgeon. https://complexspineinstitute.com/en/complex-spine-institute/en/institute/#medical_team
- Emami A. et al. Comparing clinical and radiological outcomes between single-level OLIF and XLIF: systematic review & meta-analysis (2023).
- Palacios P. et al. Efficacy and Safety of the Extreme Lateral Interbody Fusion (XLIF): meta-analysis (2024).
- Singhatanadgige W. et al. Incidence and Risk Factors for Lumbar Sympathetic Chain Injury After OLIF (2024).
- Yagi M. et al. Nationwide survey of surgical complications in lateral lumbar interbody fusion (2022).
Important notice: This content is educational and does not replace personalized medical evaluation. If in doubt or if alarm symptoms appear, consult a professional or go to an emergency department.