A clinical diagnosis on its own is unreliable. MRI can guide the assessment and rule out other causes, but confirmation in selected cases comes from diagnostic medial branch blocks. Radiofrequency can provide months of relief in patients who meet strict criteria and after appropriate conservative management. Not everyone responds, and there are risks that, while uncommon, should be understood.
- Axial low back pain that worsens with extension or twisting suggests a facet origin.
- MRI helps rule out other causes, but does not confirm facet pain by itself.
- Diagnostic blocks with strict criteria guide whether radiofrequency is appropriate.
- Radiofrequency may reduce pain for several months in selected patients.
- Start with a structured conservative plan unless there are red flags.
How does lumbar facet pain present?
It is typically an axial pain in the lower back that increases after prolonged standing, when leaning backward, or when rotating the torso, and improves with slight forward flexion. It may be accompanied by morning stiffness and tenderness on paraspinal palpation. It usually does not radiate below the knee, unlike typical sciatica. Intensity can fluctuate during the day and may worsen after exertion or sustained postures.
7 tests that truly help
- Targeted history: axial pattern, mechanical triggers, relief with flexion, and no clear neurological symptoms.
- Physical exam: pain with extension and rotation, and focal tenderness over the facet joints. Provocative maneuvers add clues, but are not definitive on their own.
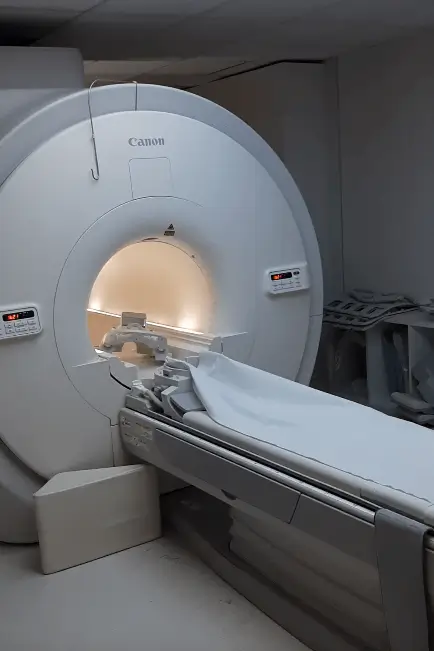
- Lumbar MRI: useful to rule out herniation, stenosis, or bone marrow edema. Facet arthrosis on imaging does not always correlate with pain, so MRI can support the suspicion but does not confirm the source.
- Dynamic X-rays: flexion-extension views to detect segmental instability when suspected.
- Diagnostic medial branch blocks: injection of local anesthetic near the medial branches that carry facet pain. Significant, reproducible relief under predefined criteria supports the diagnosis.
- Outcome measures: pain VAS and the Oswestry Disability Index (ODI) before and after interventions to track clinically meaningful change.
- Reassessment after physiotherapy: repeating the evaluation after a therapeutic exercise cycle helps refine the suspicion and the plan.
Key differential diagnosis
Painful disc degeneration, sacroiliac joint pain, myofascial pain, hip pathology, and spinal canal stenosis are common causes of low back pain. Clinical features, imaging, and, when needed, neurophysiological studies help differentiate them. For example, sacroiliac pain tends to sit lower, toward the buttock and groin, and can be supported by specific provocation tests and diagnostic injections.
Non-surgical treatment
Management is primarily conservative. It includes pain education, staying active, progressive therapeutic exercise, core strengthening, and sleep and ergonomic habits. Analgesics should be used cautiously and short term, prioritizing non-opioid options. Active physiotherapy is a cornerstone, progressing strength, motor control, and load tolerance. In selected cases, diagnostic or therapeutic injections with anesthetic, with or without steroid, can be integrated into a plan that still prioritizes exercise and functional goals.
Facet radiofrequency: when it can help
Thermal radiofrequency ablation of the medial branches aims to interrupt pain signals coming from the facet joints. It is performed under local anesthesia with light sedation and imaging guidance. The key is patient selection: compatible axial pain, failure of a well-structured conservative program, and positive diagnostic blocks according to predefined criteria. Some protocols recommend two positive blocks to reduce false positives. The goal is clinically meaningful pain relief and improved function for several months. If benefit fades over time, the procedure may be repeated, weighing the benefit-risk balance.
Benefits, limits, and risks
Expected benefits
- Pain reduction and functional improvement in a proportion of well-selected patients.
- Outpatient procedure, with a quick return to light activities.
- Can be repeated if there was clear benefit and the pain returns.
Limits and considerations
- Not everyone responds; failures may reflect mixed pain generators or overly loose selection criteria.
- Relief is usually temporary and varies between individuals.
- Lack of sustained benefit should prompt a review of the diagnosis and the plan.
Risks and adverse effects
- Temporary local pain or bruising at the needle entry site.
- Uncommon infection, vasovagal reaction, neuritis, or short-lived numbness.
- Major complications are rare when a standardized technique with imaging guidance is used.
Practical referral criteria
- Limiting axial low back pain despite 6-12 weeks of structured conservative management.
- Imaging that rules out causes requiring a different primary strategy.
- Diagnostic medial branch blocks with clinically meaningful relief under defined criteria.
- Controlled comorbidities and realistic expectations about benefits and limitations.
Realistic recovery timelines
After radiofrequency, most people return to light activity within 24-72 hours. A mild increase in local soreness is common during the first few days. When effective, meaningful improvement is usually noticed between weeks 2 and 6. Returning to work depends on physical demands, with a typical range of 3-10 days for office-based roles. Keeping the exercise program is key to prolonging benefits.
When to seek urgent care
Persistent high fever, severe and progressively worsening pain that does not improve with usual medication, rapidly worsening weakness or numbness, or new neurological symptoms after the procedure require urgent medical assessment.
Myths and facts
- Myth: radiofrequency cures any low back pain. Fact: it can help only in well-selected facet-mediated pain and as part of an active plan.
- Myth: if MRI shows facet arthritis, the pain must be facet-related. Fact: imaging does not always match symptoms, which is why diagnostic blocks matter.
- Myth: after an injection or radiofrequency, exercise is no longer necessary. Fact: therapeutic exercise remains the foundation of treatment.
Frequently asked questions
Is radiofrequency permanent?
No. It may provide months of relief and, if it worked and pain returns, it can be repeated depending on clinical course and medical criteria.
Does the procedure hurt?
It is done with local anesthesia and light sedation. There may be temporary local discomfort in the days afterward.
Do I need two diagnostic blocks beforehand?
Some protocols require two positive blocks to reduce false positives. It depends on local practice and the guidelines being followed.
Does it work if my pain goes down the leg?
If sciatica from nerve root compression is predominant, facet radiofrequency is not the main option.
What if I do not improve?
The diagnosis is reviewed, the active plan is reinforced, and other pain sources or treatment alternatives are considered.
How many times can it be repeated?
If benefit was clear but temporary, it can be repeated when pain returns, considering cumulative risks and cost-benefit.
Glossary
Facet joints: small posterior joints that stabilize each spinal level.
Medial branches: nerves that carry sensation from the facet joints.
Diagnostic block: targeted anesthetic injection to check whether pain decreases.
Radiofrequency ablation: technique that applies controlled heat to interrupt pain signaling.
References
- Dr. Vicenç Gilete – Neurosurgeon. Institute. https://complexspineinstitute.com/en/complex-spine-institute/en/institute/ (2025)
- Dr. Augusto Covaro – Orthopedic surgeon and traumatologist specializing in spine. Institute. https://complexspineinstitute.com/en/complex-spine-institute/en/institute/ (2025)
- NICE. Low back pain and sciatica in over 16s: assessment and management. https://www.nice.org.uk/guidance/ng59 (2016, updated 2020)
- ASIPP. Comprehensive Evidence-Based Guidelines for Facet Joint Interventions in the Management of Chronic Spinal Pain. https://asipp.org/wp-content/uploads/2020/11/REF1MA1.pdf (2020)
- NASS. Diagnosis and Treatment of Low Back Pain Clinical Guidelines. https://www.spine.org/Portals/0/Documents/ResearchClinicalCare/Guidelines/LowBackPain.pdf (2020)
- Cochrane Review. Radiofrequency denervation for chronic low back pain. https://www.cochrane.org/evidence/CD008572_radiofrequency-denervation-chronic-low-back-pain (2015)
- Cohen SP et al. Consensus practice guidelines on interventions for lumbar facet joint pain. https://pmc.ncbi.nlm.nih.gov/articles/PMC7362874/ (2020)
This content is educational and does not replace an individual medical evaluation. If you have warning signs or concerns, consult a qualified healthcare professional.